CSO Corner Volume 9: Making More Sophisticated Models
Hello fellow members of our KS family!
In my last article, I talked about the basic concept of making models to better understand a rare disease like Kleefstra syndrome (KS), and why we have created our own cell lines to share with researchers. I also talked about the value of induced pluripotent stem cells (iPSCs) and how they can be turned into neurons and studied in a dish. This time, I’d like to delve a little more deeply into the types of KS models that we expect to be making in the near future, and why we think they will help build the path to a treatment.

In the past, model systems have usually been based on animals, and usually that meant mice. And mice have been, and will continue to be, important models in studying diseases like KS. Like us, they are mammals, and have a similar overall body plan, organs, etc. However, there is a profound tension in using animals to model human diseases, and it is obvious: at a genetic and cellular level, while very similar, animals aren’t humans. There is a long-running joke in the research world that most diseases have been cured multiple times in mice, so if we were
veterinarians, we would be doing a spectacular job! But in many cases, those treatments failed somewhere along the way to translation into people, sometimes in (very costly) late failures in clinical trials.
Ideally, we would model human diseases in human cells. But in the iPSC neuron route, there is the opposite challenge to that of mice: though the cells are human, the environment of a dish is not natural. Studying isolated neurons in a dish does have tremendous value, and has enabled many breakthroughs. Just as with mice, it will continue to be an important method to model diseases like KS.
But, could we create systems that are more natural, and that more completely model the environment of a human brain, using human cells? There has been lots of work done by researchers over the past few years to do exactly this. For starters, the human brain doesn’t just contain neurons. It contains many other types of cells that have multiple roles, including support, immunity, etc. One route to a more complete model is to derive multiple types of brain cells from the iPSC lines, and then mix them together in the dish to provide a more natural environment.
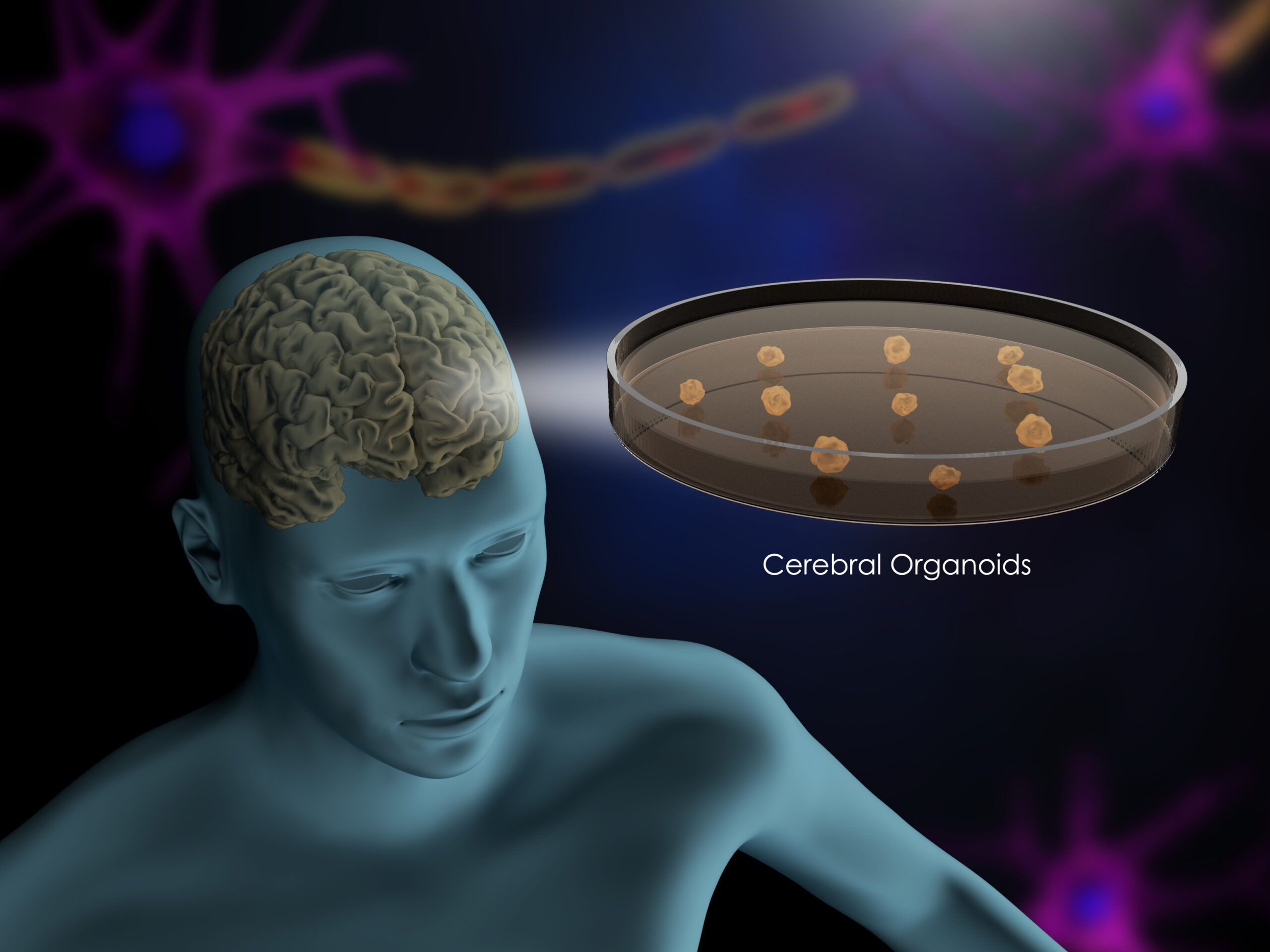
It has also been found that, coaxed in the right way, iPSCs can be made to grow into tiny structures called organoids that mimic many of the structures, and the different cell types, of a developing brain. Organoids have taken off as an approach as a result, and have been used to study many disorders.
Using these more complex model types, scientists can better understand how the brain of someone with KS may differ from that of a neurotypical counterpart, at a deep biological level. This improved understanding of mechanisms, and the interplay of the different brain cell types in those mechanisms, can open the door to potential treatment avenues. Although these technologies are young, the hope is that they will lead to more successful drug development, with a higher success rate when translated into the clinic.
In the near future, we will be announcing some new initiatives using more complex models to like those above to study KS. Stay tuned!
Until next time,
Eric Scheeff, PhD
IDefine Chief Scientific Officer

